 OVERVIEW:
OVERVIEW:
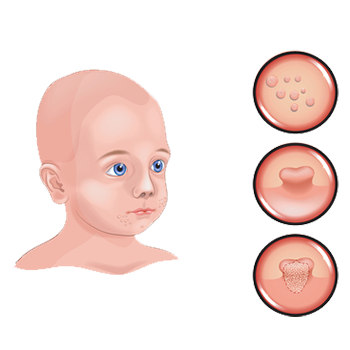
Molluscum, or molluscum contagiosum, is a common viral skin infection caused by the molluscum contagiosum virus (MCV), a virus in the poxvirus family.
This benign condition typically presents with pink, round bumps with a central indentation. The number of bumps can range in number (few to hundreds) and in size (1-6mm). The bumps can appear anywhere on the skin but prefer warm and damp environments such as armpits, areas behind the knees, crooks of the arms, and groin areas.
Occasionally, patients can develop an eczema-like rash around their molluscum bumps. Known as molluscum dermatitis, the rash is typically pink, scaly, and itchy.
Molluscum typically resolves and goes away on its own, even without treatment. As the immune system mounts a response to fight off the skin virus, the pink round bumps can become red, inflamed, and crusted.
Who Gets Molluscum Contagiosum?
Molluscum contagiosum most frequently affects young children between the ages of 1 and 10. Because of abnormalities in their skin barrier function, children with eczema seem particularly predisposed to getting molluscum.
In teenagers and adults, molluscum contagiosum most frequently presents as a sexually transmitted infection, with lesions noted in the groin region. Patients who have compromised immune systems, such as those with HIV, may be particularly susceptible to widespread molluscum contagiosum infections.
Molluscum contagiosum is contagious and can spread from one part of the body to another (auto-inoculation) through scratching or shaving. It can also spread from one person to another. It can spread through direct skin to skin contact, contact with contaminated objects (unwashed towels, sports equipment, etc), or sexual transmission. Transmission appears to be higher in wet conditions such as at the swimming pool.
How is a Molluscum Contagiosum Diagnosed?
Any new, unusual, changing, or symptomatic growth should prompt a visit to your dermatologist.
At your visit, your dermatologist will evaluate your skin and any lesions or growths of concern. Dermatologists can typically diagnose molluscum contagiosum with a skin exam. Occasionally, a skin biopsy (a procedure that removes a small sample of the skin) is done to confirm the diagnosis.
Common Treatments for Molluscum
For most individuals with a healthy immune system, the lesions of molluscum will resolve on their own even without treatment. Resolution typically occurs within 6 to 12 months, but can take up to 4 or 5 years for some. Your dermatologists may recommend letting your body clear the infection on its own rather than pursuing treatment.
For patients with symptomatic or bothersome lesions or patients with other conditions (eczema, HIV, weakened immune system), treatment may be recommended.
Common Treatment Options for Molluscum Contagiosum Include:
- Cantharidin
Derived from the blister beetle, a topical called cantharidin can be applied to the surface of the molluscum bump. Typically, the topical is left on for a period of time before it is washed off. A blister subsequently develops at the treated site. As the blister resolves, the treated lesion can crust over and peel off.
- Cryotherapy
Liquid nitrogen can be applied to freeze and destroy molluscum bumps.
- Curettage
A rounded blade called a curette can be used to scrape off the molluscum contagiosum lesions.
- Topicals Creams
Numerous topical agents have been used to treat molluscum, ranging from over the counter products to prescription medications. Examples would include: salicylic acid, imiquimod, and topical retinoids.
Talk to your dermatologist about whether or not you should pursue treatment and what treatment options would be right for you.

